If Your Baby Is Breech: External Cephalic Version (ECV)
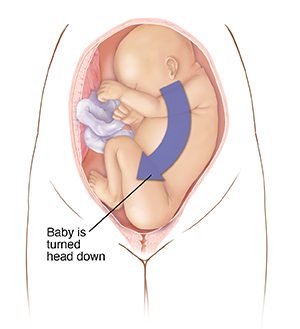
Near the end of pregnancy, most babies move into a head-down position for birth. But in some cases, a baby is in a breech position. This means the baby is upright. Their buttocks or feet are in place to come out first. A breech position makes it hard to have a vaginal birth.
If your baby is breech, your healthcare provider may press on your belly to try to turn the baby. The goal is to position your baby head-down. This procedure is called an external cephalic version (ECV). An ECV may be done if you are between 36 to 38 weeks (near term) in your pregnancy, unless there are reasons not to do it. If the ECV works well, a vaginal birth is more likely.
Before the procedure
This procedure is usually done in a hospital. Don’t eat or drink before the procedure. Follow all other directions you’re given for getting ready.
Before the ECV, the medical team will connect you to a fetal monitor. This is done to check your baby’s well-being during and after the procedure. You may also need these tests:
Ultrasound
This may be done to:
-
Confirm that the baby is in a breech position
-
Find out how much amniotic fluid is in the uterus
-
Confirm where the placenta is
-
Find or rule out any birth defects (congenital problems)
Nonstress test and biophysical profile
These tests check your baby's heart, well-being, and contraction pattern. One or both of these tests may be done before and after the ECV.
Blood tests
Medical staff will take a small sample of your blood to test. This is done to find out your blood type, screen for problems, and do a complete blood count in case of an emergency.
During the procedure
-
Your healthcare provider may use ultrasound during the procedure.
-
An IV (intravenous) line may be put in your arm. This is to give fluids or medicines if needed.
-
The team may give you medicine to relax your uterus. This can make it easier for the healthcare provider to rotate your baby.
-
You will be placed in position on the hospital bed.
-
The healthcare provider will put their hands at certain points on your lower belly over your uterus. They will press down on your belly and find your baby’s head and bottom.
-
They will try to push the baby into a head-down position. This is done by trying to make the baby do a slow-motion forward roll or back flip. You will feel pressure during this part of the procedure.
-
Once the procedure is done, the medical team will raise the head of your bed. This will help keep the baby in the head-down position.
After the procedure
-
You will stay connected to the fetal monitor. This is done to check your baby’s well-being. It also checks for contractions. These can happen after an ECV. You will be kept track of up to 2 hours after the ECV, or as noted by your provider.
-
If you are Rh-negative, you may have an Rh immunoglobulin injection. This is done to prevent an immune system response called Rh sensitization. Rh sensitization can cause problems in a future pregnancy if the baby's blood goes into your bloodstream.
-
Follow all discharge directions from your healthcare provider.
Follow-up appointments
You may need to have appointments more often to check your baby’s position.
When to call your healthcare provider
Call your healthcare provider if any of the following occur:
-
You have more contractions
-
Fluid or blood is leaking from your vagina
-
Your baby is moving less
-
You have other signs or symptoms as directed by your healthcare provider
-
You have a lot of vaginal bleeding
Delivering your baby after ECV
Even if your baby’s position can’t be changed, you may be able to have a vaginal birth. The type of birth you have should depend on your healthcare provider’s experience. Most providers prefer to do a cesarean section (C-section) for a breech baby. This is a birth done with surgery. For a C-section, you will have medicine to block pain (anesthesia). But you are usually awake and alert.
Online Medical Reviewer:
Donna Freeborn PhD CNM FNP
Online Medical Reviewer:
Heather M Trevino BSN RNC
Online Medical Reviewer:
Irina Burd MD PhD
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.