Electromyography
What is electromyography?
Electromyography (EMG) measures muscle response or electrical activity in response to a nerve’s stimulation of your muscle. The test is used to help find nerve and muscle problems.
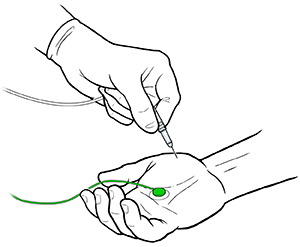
During the test, your healthcare provider will put small needles (also called electrodes) through your skin into a muscle. Sometimes, surface electrodes are used. The electrical activity picked up by the electrodes is then displayed on a monitor in the form of waves. An audio-amplifier is used so the activity can be heard. Often, several muscles are tested 1 at a time. The number and location of muscles depends on what the healthcare provider is looking for.
EMG measures the electrical activity of your muscle during rest, slight contraction, and forceful contraction. Muscle tissue does not normally make electrical signals during rest. When an electrode is put in, a brief period of activity can be seen. But after that, there should be no signal.
After the electrode is put in, you may be asked to contract your muscle, such as by lifting or bending your leg. The action potential (size and shape of the wave) that this makes on the monitor gives information about how your muscle responds to nerve stimulation. As you contract your muscle more forcefully, more and more muscle fibers are activated, making more action potentials.
A healthy muscle will show no electrical activity (no signs of action potential) during rest. It will only show it when it contracts. But if your muscle is damaged or has lost input from nerves, it may have abnormal electrical activity during rest. When it contracts, its electrical activity may make abnormal patterns.
An abnormal EMG result may be a sign of a muscle or nerve disorder, such as:
-
Polymyositis. This is an inflammatory muscle disease that causes decreased muscle power.
-
Muscular dystrophy. This is a chronic genetic disease that slowly impairs how muscles work.
-
Myasthenia gravis. This is a genetic or immune disorder that occurs at the point where the nerve connects with the muscle.
-
Myotonic (stiff) muscles
-
Damage or disease of the motor nerve, such as can be seen with nerve disease
-
Pinched nerve, such as carpal tunnel syndrome or a pinched nerve in the spine (radiculopathy)
A related test that is often done is a nerve conduction velocity (NCV). It's also called a nerve conduction study (NCS). NCV measures the speed of conduction of an electrical impulse through a nerve. NCV can determine if your nerves are damaged. It's often done during the same visit as the EMG. Both tests help find diseases that damage the nerves and muscles.
Why might I need an EMG?
EMG is often used along with NCS to tell whether you have a muscle problem or a nerve problem. NCS and EMG are best used at the same time. Together, these tests can spot disorders of the nerves, muscles, or both.
EMG may be done to find the cause of symptoms, such as muscle weakness, deformity, stiffness, and shrinkage.
EMG may be used to test for many problems, such as:
-
Motor problems, like involuntary muscle twitching
-
Nerve compression or injury, such as carpal tunnel syndrome
-
Nerve root injury, such as sciatica
-
Muscle degeneration, such as muscular dystrophy
There may be other reasons for your healthcare provider to recommend EMG.
What are the risks of EMG?
You may feel some discomfort when the needle electrodes are put into your muscles. It may feel like an acupuncture needle. Afterwards, your muscle may feel sore for a few days. A bruise may appear at the needlestick site.
The insertion of the electrodes may also cause false results on a muscle biopsy or during blood tests in which muscle enzymes are measured.
EMG may call for special precautions when done in people on anticoagulant therapy (blood thinning medicine, such as warfarin). That's because the needle electrodes may cause bleeding within the muscle.
There may be other risks based on your specific health problem. Be sure to talk about any concerns with your healthcare provider before the test.
How do I get ready for an EMG?
Ask your healthcare provider to tell you what you should do before your test. Below is a list of common steps that you may be asked to do:
-
Your healthcare provider will explain the test to you, and you can ask questions.
-
You will be asked to sign a consent form that gives your permission to do the test. Read the form carefully and ask questions if something is not clear.
-
Generally, fasting is not needed before the test. In some cases, cigarettes and caffeinated drinks, such as coffee, tea, and cola may be restricted 2 to 3 hours before testing.
-
Tell your healthcare provider of all medicines (prescribed and over the counter) and herbal supplements that you are taking, especially any blood thinners.
-
Tell your healthcare provider if you have a pacemaker or other implanted devices, such as deep brain stimulator.
-
Dress in clothes that permit access to the area to be tested or that are easily removed.
-
Stop using lotions or oils on your skin for a few days before your test, or at least stop using them on the day of the exam.
-
A sedative or pain reliever may be prescribed before the test. If so, you may need to have someone drive you home afterwards.
-
Based on your health problem, your healthcare provider may ask for other specific preparations.
What happens during an EMG?
An EMG may be done on an outpatient basis or as part of your stay in a hospital. Steps may vary based on your health problem and your healthcare provider's practices. Talk with your healthcare provider about what you will go through during your test.
The EMG is done by a healthcare provider who specializes in nerve disorders. This is often a neurologist or physiatrist.
The EMG is often done right after a nerve conduction study.
Generally, an EMG test follows this process:
-
You will be asked to remove any clothing, jewelry, hairpins, eyeglasses, hearing aids, or other metal objects that may interfere with the test.
-
If you are asked to remove clothing, you will be given a gown to wear.
-
You will be asked to sit or lie down for the test.
-
A neurologist will find the muscle(s) to be studied.
-
The skin will be cleansed with an antiseptic solution. Next, a fine, sterile needle will be put into the muscle. One or 2 wire electrodes may be placed on your skin. The same needle is often used to test several sites.
-
Several needle insertions may be needed for the test. You may have slight pain with the placing of the electrode. But it's often painless.
-
If the test is painful, tell your examiner because it can interfere with the results.
-
You will be asked to relax and then do slight or full-strength muscle contractions.
-
The electrical activity from your working muscle will be measured and displayed on the monitor. An audio amplifier may also be used so that both the look and sound of the electrical potentials can be checked. If the recorder is attached to an audio amplifier, you may hear a sound like hail on a tin roof when you contract your muscle.
What happens after an EMG?
After the test, the electrodes will be removed. You may be given pain medicine. Warm compresses may be put on the affected area right after the test.
Some muscle soreness may last for a day or so after the test. Tell your healthcare provider if you have any of the symptoms at the needle insertion sites:
-
Growing pain
-
Tenderness
-
Swelling
-
Pus
Your healthcare provider may give you other directions after the test, based on your particular situation.
Next steps
Before you agree to the test or procedure, make sure you know:
-
The name of the test or procedure
-
The reason you are having the test or procedure
-
What results to expect and what they mean
-
The risks and benefits of the test or procedure
-
What the possible side effects or complications are
-
When and where you are to have the test or procedure
-
Who will do the test or procedure and what that person’s qualifications are
-
What would happen if you did not have the test or procedure
-
Any alternative tests or procedures to think about
-
When and how will you get the results
-
Who to call after the test or procedure if you have questions or problems
-
How much will you have to pay for the test or procedure